The COVID-19 pandemic ushered in a period of unprecedented change in how we serve our patients. While the crisis caused much uncertainty for Health Services staff and our patients, Health Services leadership also viewed the pandemic as an opportunity to make positive and transformative changes to our health system.
The Population Health division of Health Services is one such team that responded to the crisis in ways that are already proving to have long-term benefits for our patients. In just a couple of weeks, Population Health implemented important changes to our health system, three of which are highlighted here: Rapid implementation of telehealth visits, chronic disease follow-up for patients fearful of COVID-19 and post-discharge follow-up for COVID-19+ patients.
Rapid Transition to Telehealth at Health Services
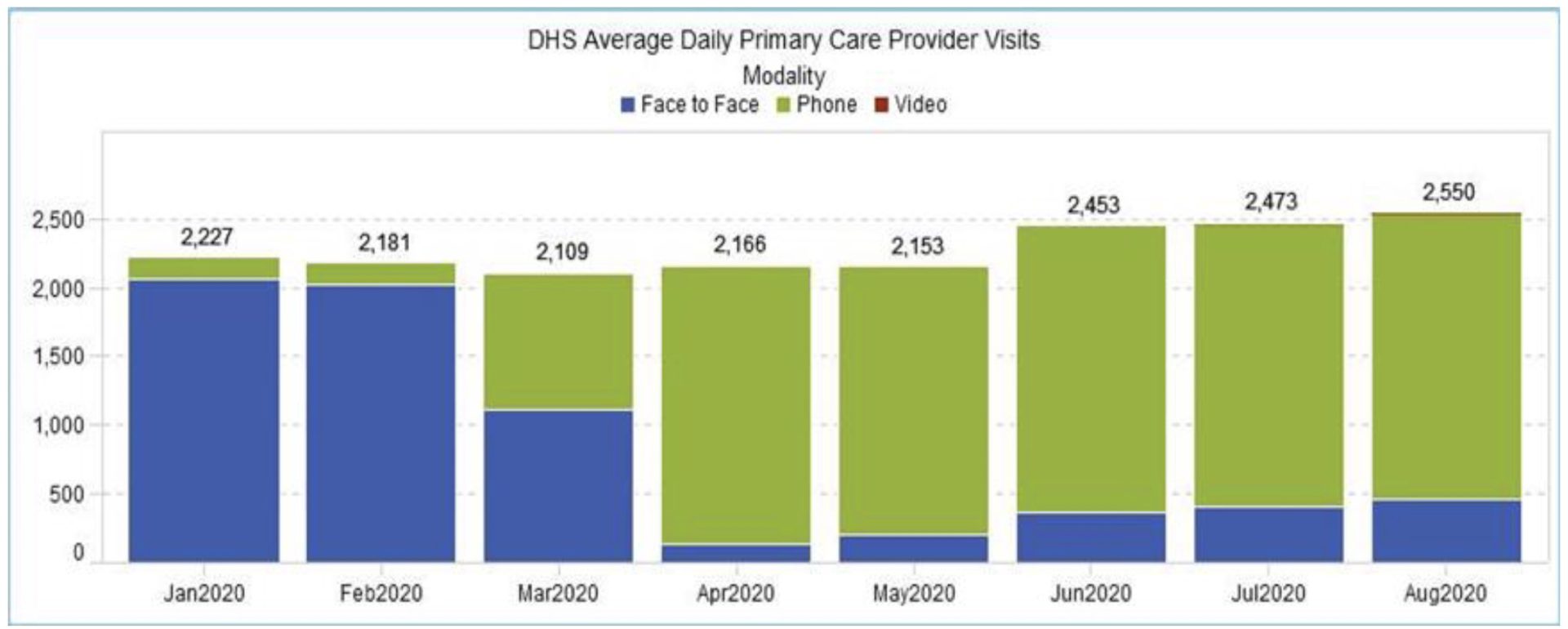
Before COVID-19, over 90% of Health Services’ primary care provider visits were conducted in-person. By April, we had flipped the paradigm, with 90% of our patients now seen through telehealth encounters. Most patient visits are completed by phone, utilizing adult and pediatric guidelines for how to conduct a team-based provider phone visit. At the same time, we have also built capacity to perform video and drive-through visits. In doing so, we haven’t just maintained access to care for our patients during this crisis, we have increased it: the average number of provider visits per day is higher now compared to pre-COVID-19 benchmarks (see Figure).
During these challenging times, every in-person interaction outside of one’s own household can place one at risk. This is especially true for higher risk Hispanic, Black, low income and medically complex patients that comprise our safety net population. During the pandemic, telehealth encounters have emerged as a critically important means to provide medical care while protecting both providers and patients from unnecessary risk. Telehealth has become a lifeline for patient care during this pandemic, and will certainly continue to serve a vital role once the pandemic is behind us.
Chronic Disease Follow-up for Patients Fearful of Contracting COVID-19
A recent New England Journal of Medicine (NEJM) perspective piece highlighted provider concern that the pandemic has caused many patients to delay essential treatments or procedures out of fear that visiting their healthcare provider might expose them to COVID-19 (“The Invisible Hand-Medical Care During the Pandemic,” NEJM April 2020). As cardiologist Dr. Michelle Kittleson explains in NEJM, many patients are experiencing a “fear of the unknown” that is preventing them from making appointments for care or proceeding with treatments.
The decision to postpone essential care comes with serious health implications for any patient, but especially for our high-risk patients living with chronic diseases. Chronic disease prevalence is highest in Hispanics, Blacks and those who are poor; Health Services manages some of the County’s most medically complex patients who carry a high burden of chronic disease. For patients living with chronic conditions, routine follow-ups are critical, and forgoing or postponing care can result in serious complications or death.
When the pandemic hit, Health Services hospitals experienced a significant drop in non-COVID Emergency Room (ER) visits and primary care teams were concerned that high-risk patients could be “falling through the cracks” and not presenting for necessary care. These patients were identified using ELM Care Management High Risk algorithms (ie. patients with diabetes, hypertension, asthma, depression, substance use and other chronic conditions) who had not had a primary care visit since March 15, 2020.
In July, primary care staff called these patients to check on how they were doing and see if they had unmet needs. Teams made between one to three outreach attempts and many sites followed up with a mailed letter. Registered Nurses, Certified Medical Assistants, Patient Access Center and Social Work staff across sites contributed to this effort which resulted in over 1,600 outreach calls. Over 700 patients were reached and more than 300 appointments were scheduled. Medications were refilled, specialty care referrals were made, and patients were connected to Social Work to assist with housing, food, and other social needs. This outreach work continues today, and feedback from patients and staff are informing Health Services on how to expand and improve patient outreach efforts moving forward.
Post-Discharge Follow-up for COVID-19+ Patients
When the COVID-19 pandemic hit hospitals throughout Los Angeles County and the nation, people saw dramatic images of ICUs and patients on ventilators, with overtaxed staff stopping at nothing to save lives. But what happens to these patients after they have survived the worst of the disease and return home? Given the unpredictability of this disease, and with so much harm done by COVID-19 to one’s body and life, the care of these patients does not end at hospital discharge.
With the goal of ensuring that no patients “fall through the cracks” after discharge from a County hospital with a diagnosis of COVID-19, the Population Health Transitions of Care (TOC) workgroup immediately implemented a new Expected Practice whereby all Health Services patients discharged with a COVID-19 diagnosis are contacted at least once, and often several times, after discharge. Each Health Services hospital created a detailed follow-up plan for their COVID-19 patients which included linking patients to an empaneled primary care provider and primary care medical home (PCMH) team if they did not already have one.
Once a COVID-19 patient leaves one of our hospitals, they will receive a call from their primary care team within 72 hours of arriving home. Patients are asked if they have a cough, fever, shortness of breath, chest pain or any other lingering effects of COVID-19. They are also asked if they have access to food or have any mental health or life concerns that need to be addressed while they recover. Family members are reminded to wear masks and wash hands frequently. And if the patient is having problems, he or she will be contacted again in a week, and possibly again the week after that.
These efforts are essential to provide both physical and moral support to our Health Services patients as they try to survive this terrible pandemic. The efforts described here are part of a broader effort within Health Services to channel the urgency and renewed sense of mission unleashed by the pandemic to rethink how we can best serve the needs of our patients amidst a dramatically altered healthcare landscape.