MD13
CASE OF THE MONTH — APRIL 2023
Case Presentation:
EMS responds to a freeway underpass where a female of unknown age was found unresponsive. Bystanders called 911 when she remained motionless despite heavy rain. On initial assessment, the patient is unconscious with a slow pulse. She is breathing spontaneously. No other history is available.
Her initial vital signs are Temp – does not register, BP 90/42, HR 42, RR 6, SpO2 93% on room air.
Multiple provider impressions are applicable. Provider impressions Altered Level of Consciousness (ALOC) and Cardiac Dysrhythmia – Bradycardia (DYSR) apply and the patient should be managed in accordance with TP-1229 – ALOC and TP-1212 – Cardiac Dysrhythmia – Bradycardia. There is also high suspicion for hypothermia since her temperature did not register and she was found down outside in the elements. The patient is bradypneic with poor tidal volume and signs of poor perfusion.
- Begin bag-mask-ventilation with 100% oxygen
- Initiate cardiac monitoring and obtain an ECG (TP-1212 – Cardiac Dysrhythmia – Bradycardia)
- Obtain vascular access
- Obtain blood glucose level
- Assess for signs of overdose (e.g. pupils, presence of drug paraphernalia)
- Administer Normal Saline for poor perfusion
- Initiate warming measures (TP-1223 – Hypothermia/Cold Injury)
- Administer Atropine 1mg (10mL) IV/I) push (TP-1212 – Cardiac Dysrhythmia-Bradycardia)
EMS begins basic airway maneuvers and starts an IV. Cardiac monitoring is initiated. Vascular access is obtained. Blood glucose is 92mg/dL.. The patient’s pupils are equal and reactive and there are no drug paraphernalia present. Normal Saline is initiated. The patient is cold to the touch with poor capillary refill and warming measures are initiated (i.e., wet clothing is removed, an emergency blanket is applied, and the patient is moved out of the cold into the ambulance).
Normal Saline is administered as well as Atropine 1mg (10mL) IV/IO.
The arrows in the ECG highlight J wave deflection often seen in hypothermia, also known as an Osborn wave or “camel-hump sign”. The J point is the point in time at the end of the QRS and onset of the ST segment. A J wave (Osborn wave) is a positive deflection at the J point.
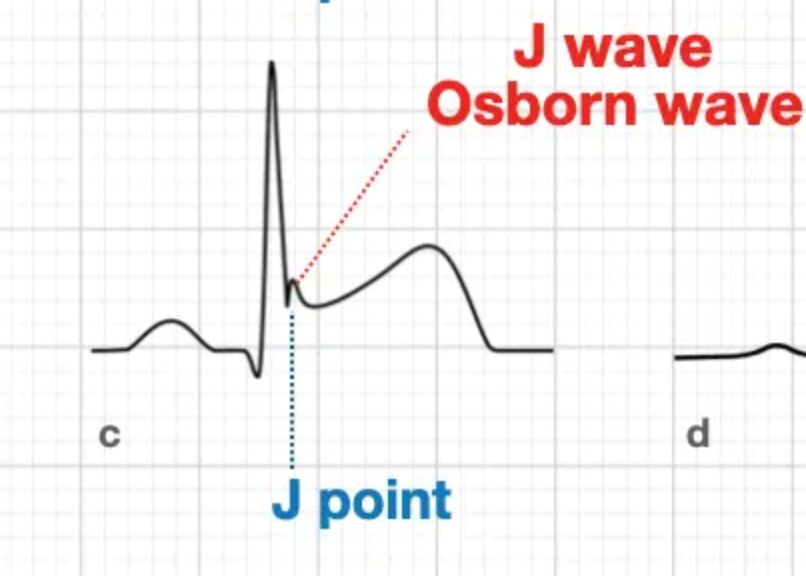
Figure 2. J wave (Osborn wave). Image obtained from https://litfl.com/osborn-wave-j-wave-ecg-library/
In hypothermia (typically below 30 degrees Celsius/86 degrees Fahrenheit), Osborn waves can be seen in conditions other than hypothermia but in the correct clinical setting, this finding can be highly suggestive of hypothermia. The height of the J wave is proportional to the degree of hypothermia.
Warming measures are continued in the ambulance. The patient’s mental status and bradycardia remain unchanged after Normal Saline and Atropine. Repeat vital signs are BP 98/48, HR 44, RR 12 (with assisted ventilation), SpO2 100% on 15L. Given the patient’s persistent poor perfusion and bradycardia, paramedics CONTACT BASE concurrently with initiation of TCP per TP 1212 – Cardiac Dysrhythmia – Bradycardia.
The underlying cause of this patient’s bradycardia is hypothermia. Hypothermia affects all organ systems, most notably the cardiovascular system and the central nervous system. Profound hypothermia will lead to decreased brain electrical activity that can mimic brain death on electroencephalogram (EEG). Similarly, hypothermia decreases depolarization of cardiac pacemaker cells, leading to bradycardia. This mechanism is not mediated by the autonomic nervous system (vagal reflex), and therefore, will not respond to atropine1. The patient’s bradycardia and mental status will not improve until she is adequately warmed.
Paramedics discuss the case with the Base. Recognizing the patient’s moderate to severe hypothermia as evidenced by physical examination (cold to touch), a temperature that will not register, and ECG findings, the Base orders that TCP not be initiated.
The patient’s clinical presentation is consistent with moderate to severe hypothermia. Bradycardia is usually physiologic in moderate to severe hypothermia, and pacing is generally not required unless bradycardia and symptoms persist despite rewarming to 32-35 degrees Celsius/90-95 degrees Fahrenheit2. The patient displays signs of poor perfusion (hypotensive, ALOC, etc.), which would usually be an indication for TCP in the setting of bradycardia, however, the underlying cause of her symptoms in this case is the hypothermia.
The patient is transported to the MAR with ongoing rewarming measures en route. Upon arrival to the MAR a core temperature reads 30 degrees Celsius/86 degrees Fahrenheit. Active external and internal rewarming is performed. The patient’s mental status improves and bradycardia resolves upon rewarming. The patient is discharged following treatment.
- Bradycardia associated with hypothermia will not respond to atropine and typically does not require pacing unless persistent after rewarming.
- J waves (Osborn waves) are found on some ECGs in hypothermic patients.
- Field management of hypothermia includes warming measures (i.e. remove wet clothing apply an emergency blanket, move the patient out of the cold).
- Li J, Alcock M. Hypothermia. https://emedicine.medscape.com/article/770542-overview#a4 accessed 3/23/2023
- Zafren K. Accidental hypothermia in adults. UptoDate updated Feb 7, 2023.
Author: Dr. Denise Whitfield, MD