CASE OF THE MONTH
CASE OF THE MONTH – OCTOBER 2021
Shots fired! Shots fired! You are called to the parking lot of a large retail store for a gun-shot wound (GSW) victim. As you arrive, several other calls have been dispatched for other patients. When you arrive, there are three patients with GSWs outside the building with reports of an active shooter. While you stage at a safe location, confirming with law enforcement that the scene is secure, panicked shoppers report that at least ten additional GSW victims are ‘down’, inside the store.
This is a Mass Casualty Incident (MCI). Given the number of reported casualties, more resources will be needed.
In accordance with Ref. No 519, Management of Multiple Casualty Incidents, you should immediately institute incident command structure (ICS) and make contact with dispatch, identifying this incident as a MCI and requesting coordination of additional resources. The Medical Alert Center (MAC) should be contacted early since 5 or more patients are involved. The MAC can contact hospitals for bed availability, determine patient destination, and establish if trauma catchment and service areas will need to be lifted to accommodate the number of traumatically injured patients. Roles and responsibilities during an MCI were summarized in a previous Emergipress on MCI Management.
Law enforcement has secured the scene and detained the shooter. Sixteen total victims have been identified from the incident as additional resources are arriving. The three initial patients found outside the building are immediately accessible for EMS assessment.
Triage protocols are summarized in Ref. No. 519.2, MCI Triage Guidelines. In Los Angeles County the modified START and JumpSTART triage tools are used.
Simple Triage and Rapid Treatment (START) is the most frequently used triage system for handling multi-casualty emergencies in the United States. START was developed in California by the Newport Beach Fire and Marine Department, along with Hoag Hospital, in the early 1980’s. JumpSTART was modified to address the needs of children.
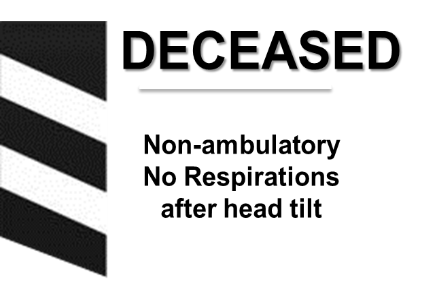
START and JumpSTART are physiologically based. According to Lou Romig, MD, the creator of JumpSTART, “patients that are unable to physiologically compensate for their injuries are assigned to a higher priority”. For children under fourteen-years-old in Los Angeles County, the JumpSTART triage system is used. JumpSTART, developed for pediatric patients in 1995, parallels the structure of START, however, it considers the unique physiology of children. Respiratory arrest is more likely in the pediatric patient population. For this reason, if there are no respirations after repositioning the airway, one should assess for a pulse in children and provide ventilations if a pulse is detected. This differs from adults where the patient would be triaged as DECEASED if there were no respirations after repositioning the airway.
START and JumpSTART are designed to complete each victim’s triage assessment within sixty (60) seconds or less. Each victim is assigned to one of four possible color categories:
- Red for Immediate and life-threatening injuries
- Yellow for Delayed victims with serious but non-life threatening injuries
- Green for Minor walking wounded/ambulatory victims
- Black for Deceased or Expectant victims that are non-breathing and/or pulseless
The primary goal of START and JumpSTART is to immediately identify patients with medical needs that can be immediately addressed to save a life.
You move to triage the first three victims utilizing the START and JumpSTART protocols.
The first victim is a 25-year-old male, carried outside by family members, with multiple GSWs to his chest. You immediately assess the respirations of this non-ambulatory victim. He has no respirations. You reposition his airway and notice that there still are no spontaneous respirations, even after you perform a head tilt and jaw thrust.
This victim is deceased. He gets a black triage tag and you proceed to assess the next victim.
The next victim is a 4-year-old female, also unable to walk. You notice that she has GSWs to her torso, as well as ecchymosis in the abdominal area. She is breathing at a rate of 46 breaths per minute.
This respiratory rate is tachypneic for a four-year-old child. Because you assessed this victim to have an abnormally high respiratory rate, she is classified as Immediate, and you move on.
Note that in triage for the pediatric patient population, when a patient has with no spontaneous respirations after repositioning the airway, JumpSTART allows the rescuer to assess for a pulse and administer ventilations. A pediatric patient with a pulse with no respirations would be categorized as Immediate.
Once you observe that this non-ambulatory pediatric victim is breathing, but at a high, abnormal rate, she immediately receives a red tag, prioritizing her for transport. It is not necessary to assess her pulse and mental status. You must move on to triage the next patient.

You turn your attention to your third victim, a 7-month-old male infant, carried in the arms of an adult caregiver. He has a GSW to his scalp. The 7-month-old infant cannot developmentally walk. You assess that he is breathing normally. Next you locate his brachial pulse, which is palpable. You finally observe that this patient is appropriate, fully awake, and alert to voice.
This pediatric victim is categorized as a green, or a minor victim and is given a green triage tag.
Any child, carried by an ambulatory adult, must be assessed separately and independently from that adult caregiver to determine their individual triage-category. The ambulatory adult may be categorized as Minor based on their ability to walk, but the pediatric victim may not be classified until a separate assessment is completed.
Another factor to consider with all pediatric patients is their developmental ability. At 7-months-old, this victim is developmentally unable to walk. He is not non-ambulatory because of sustained injuries, so he would not be categorized as “non-ambulatory” for the purpose of triage. In addition, this 7-month-old infant is non-verbal and unable to follow simple commands at baseline, therefore we assess his mental status using AVPU – is he alert to voice or pain or is he unresponsive.

The remaining 13 patients are triaged by additional EMS assets. There is one Deceased, 5 Immediate, 4 Delayed, and 6 Minor. All Immediate patients meet Trauma Criteria (4 adults, 1 pediatric) in accordance with Ref. No. 506, Trauma Triage. In coordination with the MAC, 2 adults are transported to the catchment area Trauma Center (TC) and 2 are transported to the next nearest TC, while the pediatric patient with the penetrating abdominal GSW (patient #2) is transported to the designated Pediatric Trauma Center (PTC). The remaining patients are assessed by triage priority and do not meet Trauma Criteria. They are transported to the MAR and another nearby ambulance receiving hospital for further management.
- Mass Casualty Incidents (MCIs) must be recognized early and appropriate additional resources requested.
- The primary goals of START and JumpSTART triage are to immediately identify patients with medical needs that can be immediately addressed to save a life.
- Primary respiratory arrest is more likely in pediatric patients. Therefore, for a pediatric patient lacking spontaneous respirations, JumpSTART allows the rescuer to reposition the pediatric airway, check for a pulse and to deliver ventilations if a pulse is present. A pediatric patient without ventilations and a pulse would be categorized as IMMEDIATE.
- During an MCI, any child carried in the arms of an ambulatory adult, must be assessed separately and independently from that adult to determine that child’s triage category.
Author: Millicent Wilson, MD