EMERGENCY MEDICAL SERVICES-ECG JANUARY Issue
ECG — JANUARY 2024
Case:
Paramedics respond at law enforcement request to evaluate a woman who has been acting erratically. Paramedics arrive to find a 25-year-old female who they are familiar with from recent prior psychiatric crisis calls. Today, she is laying in her bed appearing confused. Her eyes are closed. There is an empty pill bottle of diltiazem on her bed. Her initial vital signs are HR 35, BP 92/50, RR 8, SpO2 98% on room air
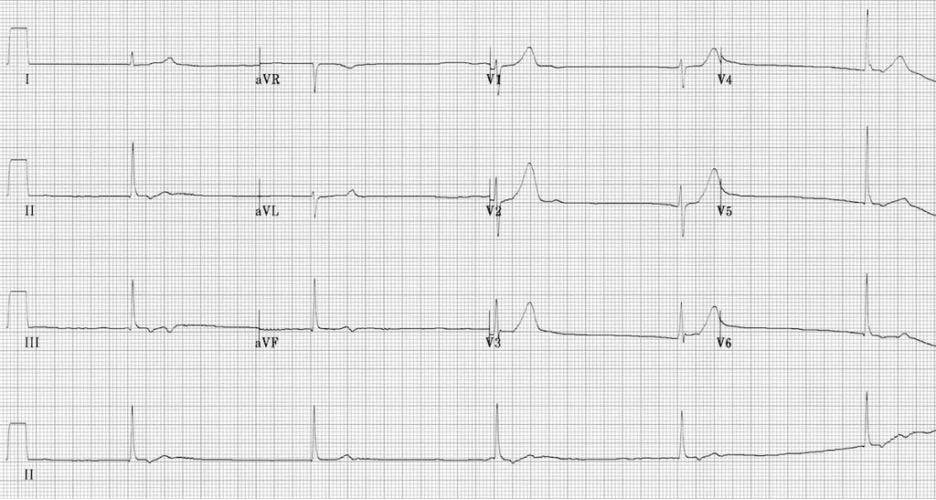
Image Source: LITFL obtained November 21st, 2023
Rate: ~30 beats per minute
Rhythm: Junctional bradycardia. No p-waves are visible. QRS complexes are narrow.
ST Segment Elevation >1mm
In 2 or more contiguous
Leads? No
Reciprocal Changes: N/A
This ECG shows a junctional bradycardia. A junctional rhythm is an abnormal cardiac rhythm that originates from the atrioventricular (AV) node or the Bundle of His. During normal cardiac conduction, pacemaker cells in the sinoatrial (SA) node generate electrical impulses causing the heart to contract. The pacemaker cells in the SA node spontaneously generate electrical impulses at a rate of 60 to 100 beats per minute (bpm). Outside of the SA node, pacemaker cells capable of independently generating electrical impulses are also found in the atrial and ventricular walls, AV node. Atrial and ventricular pacemaker cells intrinsically generate impulses at rates of <60 and 20-40 bpm, respectively, while AV node/Bundle of His pacemaker cells generate impulses at rates of 40-60 bpm.

Figure 1: Cardiac Conduction System
Image Source (no changes made): https://commons.wikimedia.org/wiki/File:ConductionsystemoftheheartwithouttheHeart.png
In a junctional rhythm, impulses from the SA node are absent or less than the intrinsic rate of the AV node (i.e. 40-60 bpm). Without electrical impulses from the SA node or atria pacemaker cells, no p-waves are visualized. In this patient, the rhythm may be classified as a junctional bradycardia given the rate is <40 bpm. There are many causes for this rhythm including cardiac ischemia, metabolic abnormalities (i.e. hyperkalemia), or drug overdose (i.e. beta blocker or calcium channel blocker overdose). Patients with this rhythm may develop signs and symptoms associated with hypotension developing from profound bradycardia including general weakness, dizziness, altered mental status, or other signs of poor perfusion.
The primary etiology of the patient’s symptoms is a junctional bradycardia likely due to a suspected overdose of diltiazem, a calcium channel blocker. Overdose of calcium channel blockers results in inhibition of cardiac smooth muscle contraction. The primary provider impression for this patient is Cardiac Dysrhythmia (DYSR) and the patient should be managed according to TP 1212, Cardiac Dysrhythmia – Bradycardia and TP 1241, Overdose/Ingestion/Poisoning. In this patient with a HR<40 bpm and signs of poor perfusion (i.e. altered mental status), Atropine 1mg (10mL) IV/IO push (MCG 1317.9, Atropine) may be attempted. If no improvement after Atropine or if unable to obtain IV access, proceeding directly to transcutaneous pacing per MCG 1365, Transcutaneous Pacing. For transcutaneous pacing, pads should be placed in an anterior (i.e. left chest)/posterior position (i.e. back). Set the initial pacing rate at 70 bpm for adults. Set the current at 40 milliamperes (mAs). Slowly increase the mAs until electrical and mechanical capture has been achieved as evidenced by a palpable pulse which correlates with the paced heart rate on the monitor. Once capture is noted, increase the mAs by 10mAs to ensure ongoing capture. If the current is increased to 120-130 mAs without capture, consider repositioning the pacer pads on the upper right chest and at the apex of the heart, and reattempt. Base contact is required for all patients with symptomatic bradycardia and concurrently with initiation of transcutaneous pacing.
For patients who are awake, providers may consider Midazolam 5mg (1mL) slow IV/IO push or IM/IN for sedation during TCP. For persistent poor perfusion after initiating TCP, consider Normal Saline 1L IV/IO rapid infusion and Push-dose Epinephrine. Contact Base to obtain an order.
The secondary provider impression in this case is Overdose/Ingestion/Poisoning (ODPO) and the patient should be managed according to TP 1241, Overdose/Ingestion/Poisoning. Base contact should be made to discuss administration of Calcium Chloride 1g (10mL) IV push over 60 seconds (MCG 1317.11, Calcium Chloride) as an antidote for suspected calcium channel blocker overdose. The proposed mechanism of action is that calcium chloride increases circulating calcium and overcomes the inhibition of cardiac smooth muscle function by calcium channel blockers. Hyperglycemia is often seen in conjunction with calcium channel blocker overdose.
The patient is transported to the MAR. On hospital ECG, the patient’s cardiac dysrhythmia progressed to a complete heart block (i.e. third degree block).
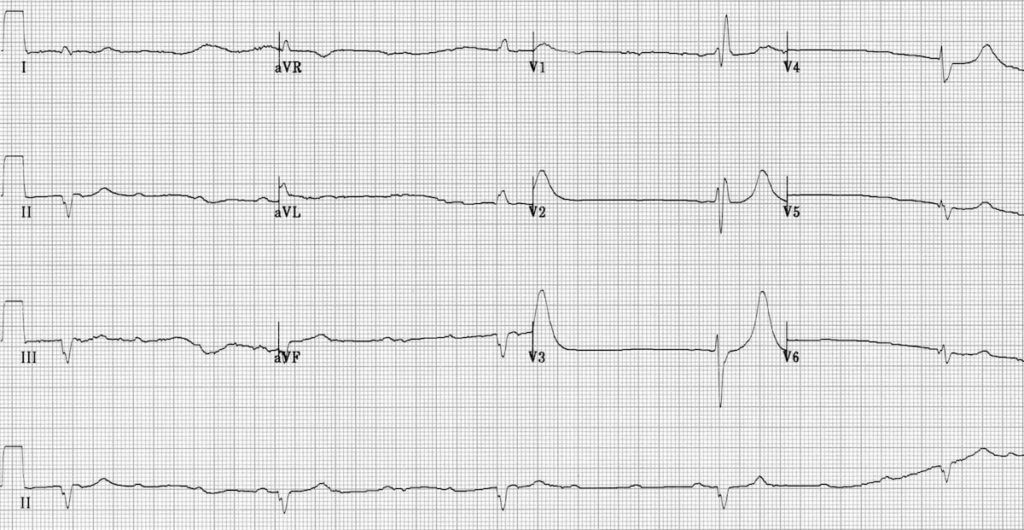
Image Source: LITFL obtained November 21st, 2023
Notice that there is no association between the p-waves and QRS complexes. The emergency department continued treatment for calcium channel overdose including continued cardiac pacing and the patient was admitted to the ICU.
Author: Jake Toy, DO, MS