EMERGIPRESS – ECG OF THE MONTH
ECG — October 2023
Case presentation
Paramedics respond to a 52-year-old male with shortness of breath and “heartburn” symptoms that started about 2 hours prior to EMS arrival. Initial vital signs on scene are BP:132/61 HR: 210 RR: 26 SpO2: 70%.
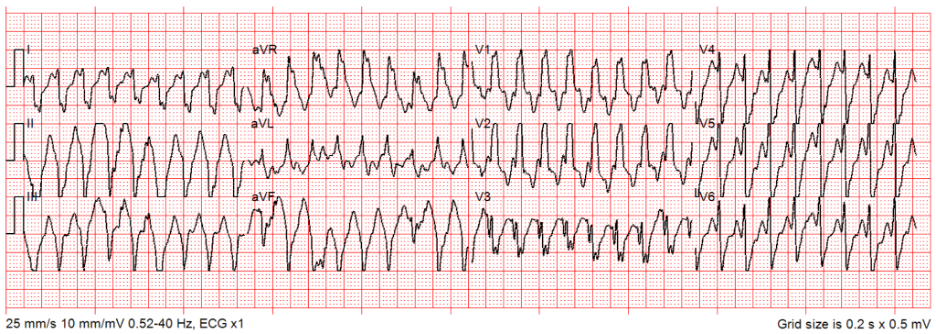
Rate: ~210 bpm
Rhythm: Regular wide complex tachycardia (> 0.12 sec), there are no p-waves before each QRS
ST Segment Elevation >1mm
In 2 or more contiguous
Leads?: N/A
Reciprocal Changes: N/A
This ECG demonstrates a regular wide complex tachycardia. Regular wide complex tachycardias can be ventricular tachycardia (VT) or supraventricular tachycardia (SVT) with aberrancy (conduction delay). Determining the difference between these rhythms can be quite challenging, even for physicians specializing in cardiology. For this reason, American Heart Association Advanced Cardiac Life Support (ACLS) guidelines do not distinguish the management of VT from SVT with aberrancy. Instead, they determine the management of tachycardic cardiac dysrhythmias based on their characteristics: narrow versus wide complex and regular/monomorphic versus irregular.
First line medication treatment for alert patients with regular wide complex tachycardia is adenosine. Adenosine is a short-acting medication that slows AV node conduction. For patients with SVT, this slowing may allow termination of re-entry conduction, allowing conversion back to normal sinus rhythm. Adenosine is not effective for patients with VT; however, administration of adenosine in a patient with VT is unlikely to cause harm if the patient is otherwise stable. Therefore, adenosine can be given for hemodynamically stable, regular, wide complex tachycardia of unknown type since it is relatively safe. Regular, wide complex tachycardia patients that are unstable (poor perfusion with altered level of consciousness) require immediate Synchronized Cardioversion to convert the rhythm and restore adequate perfusion.
This patient’s ECG shows a regular wide-complex tachycardia. The patient should be managed per TP 1213 – Cardiac Dysrhythmia – Tachycardia. It is important to recognize that cardiac dysrhythmias can present as a variety of chief complaints including, but not limited to: dyspnea, palpitations, abdominal pain, altered mental status, dizziness, nausea, and vomiting. Consider cardiac dysrhythmia for these complaints and obtain an ECG. Rapidly assessing life threats, identifying signs of poor perfusion, and treating dysrhythmias promptly can prevent further deterioration, including cardiac arrest.
For this patient, there a few things to consider:
- Are you able to establish IV access?
Depending on the perfusion status of the patient, this may determine if Adenosine can be attempted or if one should move directly to Synchronized Cardioversion. - Is the patient perfusing?
For adequate perfusion, initial treatment is Adenosine 6 or 12mg (2 or 4mL) rapid IV push. If the patient is alert with poor perfusion, Adenosine 12mg (4mL) rapid IV push can be given if vascular access is available. If there is no vascular access or no conversion with adenosine, Synchronized Cardioversion is performed. For poor perfusion with ALOC, perform Synchronized Cardioversion immediately. - Has the patient experienced a cardiac dysrhythmia before? If so, what therapy worked?
If a patient has had this cardiac dysrhythmia before and converted with adenosine, it is likely SVT with aberrancy. If the patient is alert with vascular access, this can be tried first and may be likely to respond again to this therapy. - Does the patient have an AICD? Has it fired?
Many patients at risk for ventricular cardiac dysrhythmia have an AICD implanted that will defibrillate the patient when ventricular tachycardia or fibrillation is sensed. If the AICD has fired, this likely means that a cardiac dysrhythmia was sensed.
As mentioned, this regular wide complex tachycardia could be VT or SVT with aberrancy. In this case, Adenosine may convert the rhythm to sinus and should be given for alert patients with vascular access. Adenosine should not be used for irregular wide complex tachycardia (Wolf-Parkinson-White Syndrome with atrial fibrillation) because this may lead to degeneration to a fatal dysrhythmia (ventricular fibrillation). Adenosine is also contraindicated in patients with Sick Sinus Syndrome, heart transplant, or patients taking carbamazepine (Tegretol) as noted in MCG 1317.1 Drug Referece – Adenosine.
This patient was placed on oxygen via NRB mask per MCG 1302 given their hypoxia on arrival. This improved his SpO2 to 90% while defibrillation pads were placed and IV access was obtained. The patient was alert with adequate perfusion, so the patient was given Adenosine 6 mg (2mL) rapid IV push, followed by Adenosine 12mg (4mL) rapid IV push without rhythm conversion. In consultation with base medical direction, there was concern that the patient’s rhythm could deteriorate given the rapid rate. The patient was sedated with Midazolam 5mg slow IV push and underwent Synchronized Cardioversion at 120J. After the cardioversion, the patient’s heart rate decreased to 130 bpm before further improving with fluids. He was transported to the MAR. After evaluation by cardiologists, it was determined that the underlying rhythm was ventricular tachycardia and he had an Automatic Implantable Cardioverter Defibrillator (AICD) placed.
References
- Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000916
Author: Kelsey Wilhelm MD1,2, Marcus Black FFPM 2
- Los Angeles County EMS Agency
- City of Compton Fire Department