EMERGENCY MEDICAL SERVICES-ECG02
ECG OF THE MONTH – OCTOBER 2021
Case:
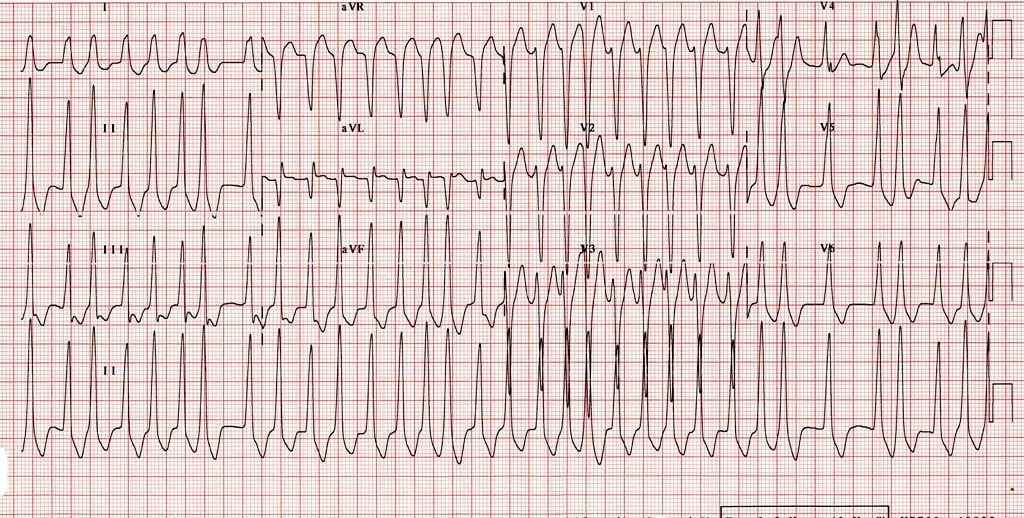
Paramedics respond to a 62-year-old male with palpitations and dizziness. He was eating breakfast when he suddenly started to feel his heart race. He is awake and alert but appears pale. His vital signs are BP 78/43 HR 190 RR 24 O2Sat 94%
ECG obtained from LITFL. https://litfl.com/pre-excitation-syndromes-ecg-library/ accessed 10/19/21
Rate: ~200 bpm
Rhythm: Irregularly, irregular without p-waves
ST Segment Elevation >1mm
In 2 or more contiguous Leads? No. Given the rapid rate, ST segments are shortening making interpretation difficult,
however no obvious ST segment elevations are seen.
Reciprocal Changes: N/A
This ECG shows a specific type of inferior ST elevation MI (STEMI) that is concerning for a right-ventricular STEMI. A right-ventricular STEMI is difficult to diagnose on a traditional 12 lead EKG because the only rightward facing ECG lead is V1. In order to diagnose a right-ventricular STEMI, you need to look for the following:
- consider a right-ventricular STEMI when you see an inferior STEMI
- ST elevations in lead III will be higher than the ST elevations in lead II
- Look for ST elevation in V1
Once you suspect a right-ventricular MI, you can obtain a right-sided EKG to confirm the diagnosis.
This ECG is consistent with atrial fibrillation with rapid ventricular response in Wolff-Parkinson-White (WPW). Notice that the rhythm is irregularly irregular, characteristic of WPW. One can also appreciate delta waves at the beginning of the QRS complexes, most clearly seen in leads II, III, and aVF. This is a wide complex, irregular, tachycardic cardiac dysrhythmia. Wide complex regular tachycardic dysrhythmias can represent ventricular tachycardia or SVT with LBBB/aberrant conduction. In this ECG, it is important to recognize that the rhythm is irregular.
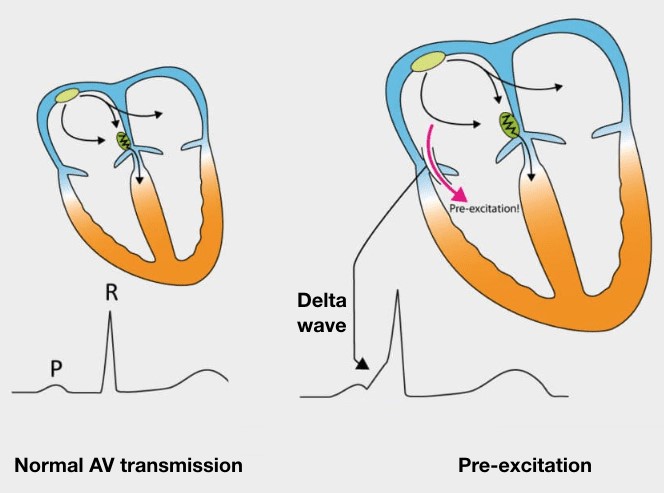
Image obtained from LITFL. https://litfl.com/pre-excitation-syndromes-ecg-library/ Accessed 10/19/21
WPW in atrial fibrillation can lead to ventricular rates greater than 200 bpm because the atrial impulses conduct down the accessory pathway rapidly. This can lead to hemodynamic instability due to the rapid rate and inability for the ventricle to fill adequately.
This patient presents with a tachycardic cardiac dysrhythmia and should be treated in accordance with TP-1213 – Cardiac Dysrhythmia – Tachycardia. The patient is in atrial fibrillation, but also has WPW leading to a wide-complex irregular rhythm. The Wide-Complex – Irregular section of TP-1213 should be followed. If the patient is adequately perfused, CONTACT BASE for treatment guidance. Adenosine is contraindicated in patients with wide-complex, irregular cardiac dysrhythmias whereas adenosine would be indicated if the patient had a regular/monomorphic wide-complex rhythm. Giving adenosine to a patient in atrial fibrillation with WPW can lead to the rhythm degenerating into ventricular fibrillation, a fatal dysrhythmia. Adenosine is a nodal blocking agent. In cases of atrial fibrillation with WPW, if the nodal pathway is blocked, all electrical impulses will propagate through the accessory pathway. Given the rapid atrial impulses in atrial fibrillation, unopposed rapid propagation through the accessory pathway can result in ventricular fibrillation. This is why recognition that the rhythm is irregular is important.
In this case, the patient is hypotensive and pale which are signs of poor perfusion. Synchronized Cardioversion at 120J is indicated. One should CONTACT BASE concurrently with cardioversion. Midazolam sedation may be given at provider discretion prior to cardioversion if the patient is awake and alert, despite the hypotension.
This patient was cardioverted prior to transport and returned to a normal sinus rhythm with resolution of symptoms. He was admitted to the cardiology service for further evaluation.
References
Burns, E. and Buttner R. Pre-excitation syndromes. https://litfl.com/pre-excitation-syndromes-ecg-library/. Accessed 10/19/21.
Author: Denise Whitfield, MD, MBA