EMERGENCY MEDICAL SERVICES-Issue7
ECG of THE MONTH — April 2022
|
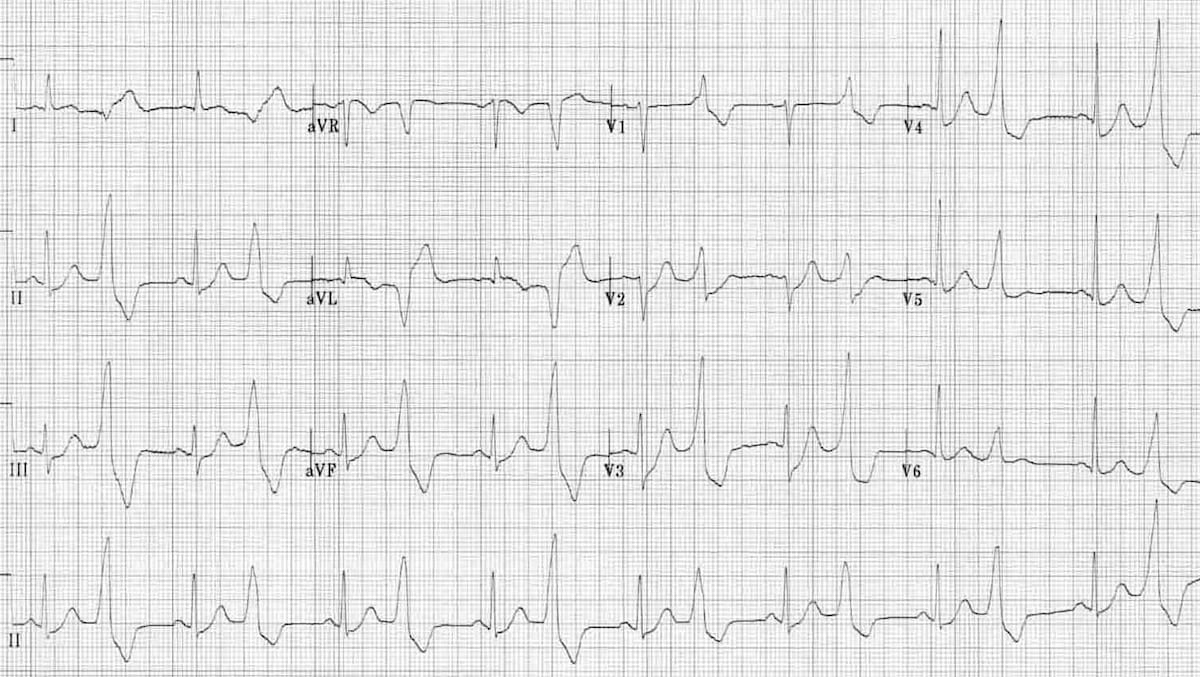
Case: Paramedics respond to a 54-year-old female whose daughter called EMS when the patient described an intermittent feeling of her heart “skipping a beat”. Her past medical history includes diabetes, hypertension, and obstructive sleep apnea. Current medications include metformin, lisinopril and hydrochlorothiazide. She is asymptomatic when EMS arrives.
Image Source: Life in the fast lane (LITFL), Premature Ventricular Complex. https://litfl.com/premature-ventricular-complex-pvc-ecg-library/ Accessed March 21, 2022 |
Rate: ~96bpm (using 10 second rule)
Rhythm: Normal Sinus Rhythm (there are p-waves before each sinus beat QRS),
with frequent premature ventricular contractions (PVCs) occurring
in “every other beat” pattern
ST Segment Elevation >1mm
In 2 or more contiguous
Leads?: No
Reciprocal Changes: N/A
This ECG demonstrates ventricular bigeminy. Ventricular bigeminy is defined by alternation of normal sinus beats and premature ventricular complexes (PVCs). A PVC is a premature beat originating from an ectopic focus within the ventricle. This ectopic electrical activity bypasses the His-Purkinje system causing asynchronous contraction of the ventricles, as seen on ECG as widening and abnormal morphology of the QRS complex. The most common causes of PVC’s include stressors that cause enhanced automaticity including electrolyte imbalances, drugs (cocaine, methamphetamines, caffeine), ischemic damage (myocardial infarction), electrolyte abnormalities (e.g., potassium, magnesium) and increased sympathetic activity (anxiety, etc.).
Examining the QRS complex in lead V1 can help discern the location of the ectopic focus. If the electrical conduction originates in the right ventricle, you will see a LBBB pattern with a dominant S wave, like in this case’s ECG. If the electrical conduction originates in the left ventricle, you will see a RBBB pattern with a dominant R wave.
When taking a closer look at the rhythm strip you can note the rate is regular although the T-P interval is extended after each PVC. This is a phenomenon known as a compensatory pause. A compensatory pause can be seen if the PVC conducts as an early after depolarization (EAD). This early depolarization allows for increased time between ventricular beats resulting in greater filling of the ventricles. The increased preload will cause increased wall stretch causing a stronger contraction, which results in the feeling of palpitations in the patient.
This patient is currently asymptomatic but endorsed palpitations prior to EMS arrival and bigeminy is seen on ECG. Attention to detail should be placed on patient history for possible precipitating factors including prior or active MI, medications, substance abuse and stressors. With this information, inspect the ECG for signs of ischemia or other changes that may be an underlying cause of the bigeminy, which may be intervened upon. In general, bigeminy is a benign ECG pattern that does not warrant additional EMS treatment. In very rare cases, this arrhythmia may evolve into or trigger the onset of a re-entrant tachydysrhythmia, including atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia AVRT), ventricular tachycardia or ventricular fibrillation. AVRT which involves a concealed bypass track is by far the most common mechanism for supraventricular tachycardia (SVT) in children, whereas AVNRT is the most common mechanism for SVT for adults. PVCs are common in all age groups but far more common in the adult patient. Monitor for signs and symptoms of change in rate or rhythm including chest pain, palpitations, shortness of breath or decreased responsiveness. This patient’s provider impression is, Palpitations (PALP), and she should be treated in accordance with TP-1202, General Medical. Initiate cardiac monitoring and transport.
The patient was transported to the Most Accessible Receiving (MAR) where patient evaluation did not demonstrate any signs of acute ischemia or electrolyte abnormalities. The patient was discharged home with primary care and outpatient cardiology follow up to evaluate for any cardiac structural abnormalities.
References
- Burns E, Buttner R. Premature Ventricular Contractions. Life in the fast lane Life in the Fast Lane, , 2008. https://litfl.com/premature-ventricular-complex-pvc-ecg-library/ Accessed March 21, 2022.
- Marcus GM. Evaluation and Management of Premature Ventricular Complexes. Circulation. 2020 Apr 28;141(17):1404-1418.
- Antonis S Manolis, MD. Premature ventricular complexes: Clinical presentation and diagnostic evaluation. Uptodate. Feb 2022.
Author: Brad McIntyre, MD, PharmD