EMERGENCY MEDICAL SERVICES (EMS) AGENCY-ECG08
ECG OF THE MONTH – JUNE 2023
Case Presentation:
Paramedics respond to a 2-year-old male with resolved tonic-clonic activity and loss of consciousness. Parents called EMS when the patient started to shake and became unresponsive. Initial vital signs are Temp 102.5 F BP 90/58 HR 165 RR 26 SpO2 97%.
dhs content/Home/More Health Services/Departments/Emergency Medical Services/Emergi Press/ECG08/InformationInformation
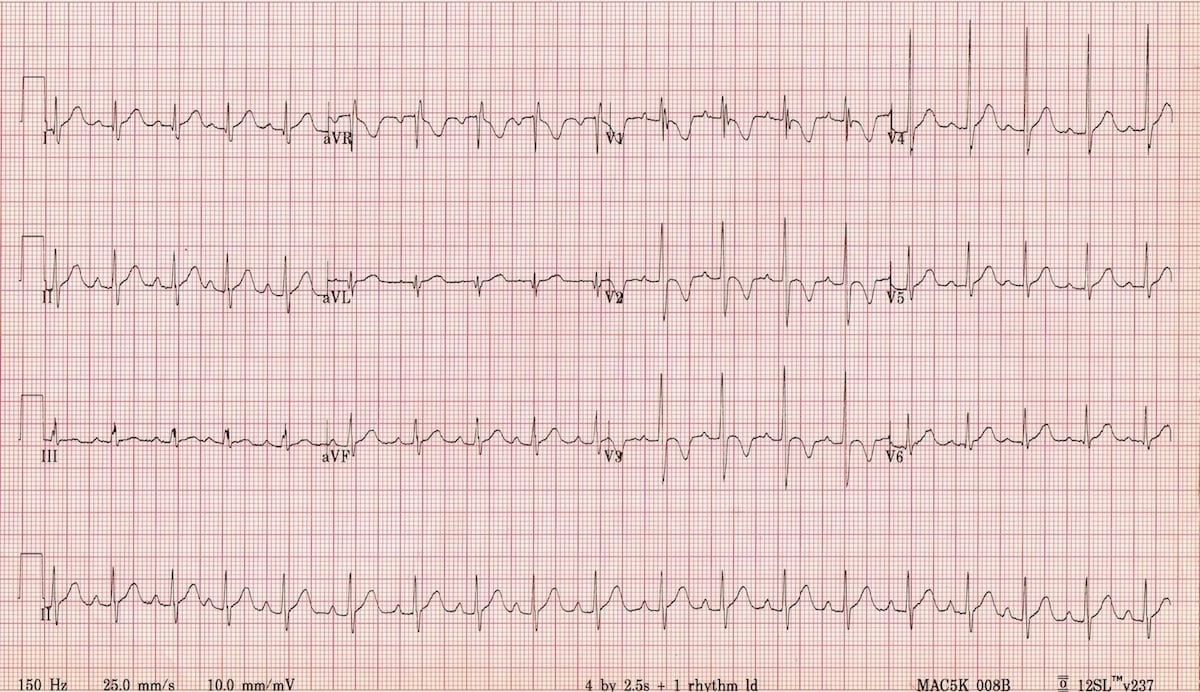
Image Source: LITFL obtained 5/23/23
Rate: 120 bpm
Rhythm: Sinus rhythm, there is a p-wave before each QRS
ST Segment Elevation >1mm
In 2 or more contiguous
Leads?: N/A
Reciprocal Changes: N/A
This ECG demonstrates a normal pediatric ECG. In this case, paramedics obtained an ECG due to the tachycardia noted on the monitors and the patient’s change in mental status on initial assessment. Although the final diagnosis was a simple febrile seizure, syncope was considered in the setting of initial tachycardia, so an ECG was obtained.
Pediatric ECGs typically have some findings that we consider abnormal when found in adults but are completely normal for children. An example of this in this ECG are the t-wave inversions in anterior leads V1, V2, V3. In adults, this is concerning for cardiac ischemia. But in children, this is known as a “juvenile t-wave pattern”. The t-wave will become upright as the child ages with 50% of 3-5 year old children having an inverted t-wave in lead V2 and only 5-10% having this finding by age 8-121.
Inverted t-waves in all the precordial leads (V1-V6)would be considered abnormal and cause for concern as would a QTc interval >.44 seconds in boys and >.46 in girls. A QTc>.50 seconds is a significant risk for life threatening dysrhythmias such as Torsades de Pointes2.
Other findings common in children is a heart rate > 100 which may be normal for age, shortened PR and QRS intervals ,and an rSR’ pattern in V1 that mimics a right bundle branch block (as seen in this ECG). The incomplete right bundle branch block pattern occurs because the size of the right ventricle is relatively large in children compared to adults. This pattern resolves as the child ages and the left ventricle becomes larger.
One finding that is quite common in pediatric ECGs is a respiratory sinus arrhythmia where the heart rate fluctuates with breathing. This may appear to be an abnormally irregular rhythm, however there is a p-wave indicating that it is a sinus rhythm. The variation is due to intermittent parasympathetic activation (vagus nerve) with breathing that results in variation in the resting heart rate.
This patient’s ECG is normal and does not suggest a current cardiac dysrhythmia. Given the history of tonic-clonic activity and the patient having a fever, a simple febrile seizure is most likely, and the patient can be managed in accordance with TP 1231-P, Seizure.
References
- Dickson, DF. The normal ECG in childhood and adolescence. Heart. 2005;91(12): 1626–1630
- Al-Akchar M; Siddique MS. Long QT Syndrome, Stat Pearls December 2022. https://www.ncbi.nlm.nih.gov/books/NBK441860/
Author: Denise Whitfield, MD, MBA