EMERGENCY MEDICAL SERVICES (EMS) AGENCY- CE35
ECG of The Month —April 2023
Case:
Paramedics respond to a 49-year-old female with a history of hypertension and a “heart problem”. Her daughter called 911 when the patient had difficulty getting out of bed in the morning. The patient is awake and alert with normal skin signs. She is unable to answer questions but appears anxious. Vital signs are BP 138/82 HR 173 RR 25 SpO2 96%.
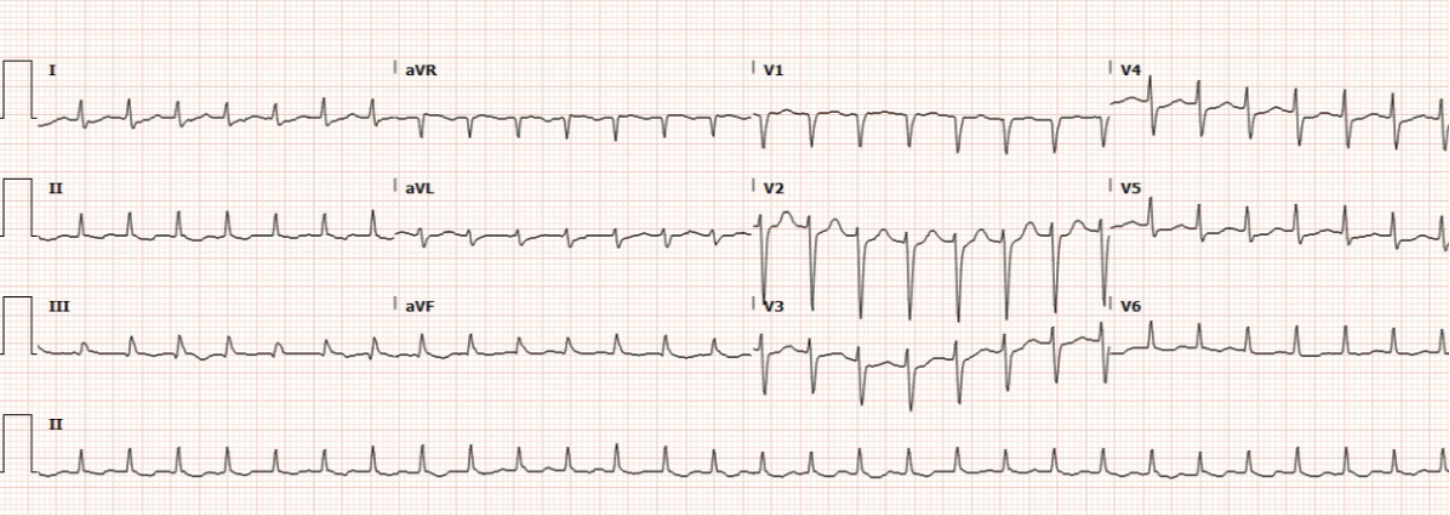
Rate: 170 bpm
Rhythm: Supraventricular tachycardia (SVT) with narrow complex; there are no p waves before each QRS
ST Segment Elevation >1mm
In 2 or more contiguous
Leads?: No
Reciprocal Changes: N/A
This ECG demonstrates supraventricular tachycardia with a narrow complex. Supraventricular tachycardia is a term that refers to any tachydysrhythmia that initiates above the Bundle of His. Most commonly it is used to refer to one form of SVT known as AV nodal re-entrant tachycardia (AVNRT). Patients with AVNRT often have accessory pathways that allow conduction from the ventricle back to a site of origin above the Bundle of His, leading to a tachycardic dysrhythmia.
Patients with SVT may be asymptomatic, feel palpitations or demonstrate signs of poor perfusion due to poor cardiac output (the tachycardic heart rate can lead to impaired ventricular filling). Patient symptoms determine field treatment in accordance with TP 1213 – Cardiac Dysrhythmia – Tachycardia.
This patient has SVT – Narrow Complex. She is normotensive with adequate perfusion given that she is awake and alert with normal skin skins. For SVT – Narrow Complex patients with adequate perfusion, attempt Valsalva maneuver. If Valsalva maneuver is ineffective, Adenosine 6 or 12mg (2 or 4mL) rapid push is given. If no cardioversion after Adenosine 6 or 12mg (2 or 4mL), Adenosine 12mg (4mL) is given.
One Valsalva technique is the modified Valsalva. The REVERT trial was a randomized control trial published in 2015 that showed a 43% success rate with this technique compared to 17% with standard Valsalva. With this technique a patient is placed in Semi-Fowler’s position with the head elevated to 45 degrees. The patient blows into a 10cc syringe for 15 seconds with instructions to blow hard enough to move the syringe plunger. After 15 seconds, lower the head of the bed so the patient’s head is flat and raise their legs for 15 seconds. Return the patient to Semi-Fowler’s position and assess the rhythm. This should only be performed in patients with adequate perfusion.
This patient has SVT – Narrow Complex with adequate perfusion at this time. She should have a Valsalva maneuver performed. A modified Valsalva is performed.
Following the modified Valsalva, this patient cardioverts to normal sinus rhythm:
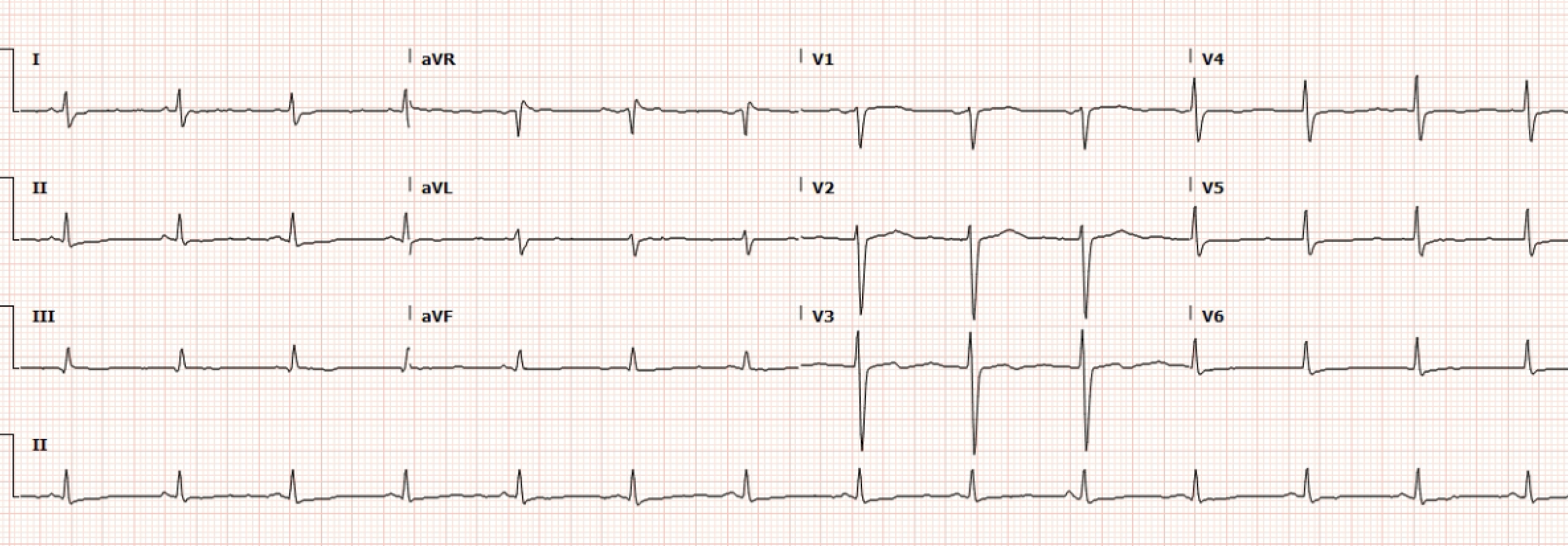
Figure 2. Normal Sinus Rhythm following Synchronized Cardioversion.
The post-cardioversion ECG demonstrates no signs of STEMI. The patient is transported to the MAR.
Author: Denise Whitfield, MD, MBA