CASE FROM THE FIELD – APRIL ISSUE
CASE OF THE MONTH – April 2021
Case Presentation:
EMS providers respond to the home of a 31-year-old male who is unresponsive after reportedly snorting an unknown amount of a powdered substance. Upon arrival, a concerned friend ushers paramedic into a bedroom to find a man lying next to a mattress, unresponsive. The friend states that the patient purchased what he thought was cocaine from a new dealer and snorted an unknown amount approximately 20 minutes prior. When he would not wake up, the friend called 911. The friend reports that this has happened before when his friend’s cocaine was allegedly cut with fentanyl. There is an open bag with a residual white substance as well as a powdered white substance on the mattress next to the patient. On initial assessment, the patient has agonal respirations and does not respond when you call his name. Initial vitals are BP 100/65, HR 62, RR 5, O2 Sat 86% on room air. He has pinpoint pupils.
Provider safety is first priority. Given that the open bag may contain an illicit substance, the EMS providers should ensure proper PPE. The National Institute for Occupational Safety and Health (NIOSH) recommends nitrile gloves, gown, respiratory protection, and eye protection for responders that may come into contact with any unknown illicit substances, including fentanyl1. Additionally, in 2017 the American College of Medical Toxicology and American Academy of Clinical Toxicology provided recommendations for first responder PPE specifically in the setting of suspected opioid overdose. These experts concluded that it would be highly unlikely for first responders to develop opioid toxicity from incidental contact with opioids, including fentanyl powder, during routine care because transdermal exposure to small amounts of powdered opioids is unlikely to cause toxicity2. If a suspected powdered opioid does contact a responder’s skin, it should be brushed off. In unusual circumstances of significant airborne suspension of powdered opioids (i.e., large drug manufacturing operations) or risk of splashes to the face, a properly fitted N95 and eye protection would be indicated. These basic PPE measures are sufficient to keep EMS providers safe from developing opioid toxicity due to a line of duty exposure. In the extremely rare event of poisoning after exposure, naloxone should be administered for objective signs of hypoventilation or altered level of consciousness (not vague concerns of dizziness or anxiety)2.
This patient presented with altered level of consciousness after a possible opioid overdose. His primary provider impression is Overdose/Poisoning/Ingestion (ODPO) given confirmed illicit drug ingestion, with a high likelihood of opioid overdose. His altered level of consciousness, hypoventilation/apnea and pinpoint pupils are all clues that point to opioid overdose. One may use ALOC – Not Hypoglycemia or Seizure (ALOC) as a secondary provider impression since the likely underlying cause is known. The patient should be managed in accordance with TP-1241, Overdose/Poisoning/Ingestion. The initial steps in management include assessment of airway and basic airway maneuvers as well as administration of oxygen as needed. Naloxone should be administered via the IN, IM or IV route (Table 1). Administration should not be delayed while vascular access is established.
Adult Naloxone Dose
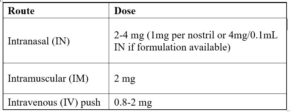
*Max dose is 8 mg for all routes prior to Base Contact. Contact base if partial response to naloxone for additional doses. Titrate to approximate RR of 12 and adequate tidal volume.
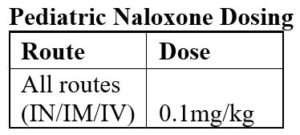
*Max dose is 8 mg for all routes prior to Base Contact. Contact base if partial response to Naloxone for additional doses. Titrate to approximate RR of 12 and adequate tidal volume.
Assisted positive pressure ventilation via bag-valve mask is initiated. After ventilations are established, Naloxone 4 mg IN is administered. After administration of naloxone, a complete assessment is performed. On initial exam, the patient has shallow respirations with a rate of 5 and a GCS of 3. Within 2 minutes of naloxone administration, his respirations increase to 8 but continue to be shallow, and his GCS improves to E1,V2, M4. Repeat vital signs are completed after the first naloxone dose with BP 112/70, HR 72, RR 9, O2 Sat 100% on 15L via NRB.
After administration of naloxone, close monitoring is important because symptoms can recur once the naloxone wears off. In particular, attention should be given to respiratory status as respiratory failure leading to cardiac arrest is the primary cause of death in opioid overdose cases. Of note, the goal of prehospital naloxone therapy is to produce a normal RR ≥ 12 with adequate tidal volume.
Conversely, naloxone administration can also precipitate sudden opioid withdrawal. In these cases, supportive care is indicated. EMS providers should be aware that patients may become agitated or combative. One’s approach to the patient should be as calming as possible. Additional doses of opioids such as morphine or fentanyl should not be administered.
After the initial Naloxone 4mg IN dose, the patient continues to have shallow respirations, RR 10. He has shallow tidal volumes with a persistent GCS 7.
An additional dose of Naloxone is indicated and a second dose can be given per TP-1241, Overdose/Poisoning/Ingestion. EMS providers should contact the base hospital if more than 8mg of naloxone is needed. If a clinical effect does not occur after 5 – 10 mg, other etiologies of altered mental status should be considered.
EMS providers initiate ETCO2 monitoring in accordance with MCG 1305, Capnography and it reads 57 mmHg. A second dose of naloxone is given. Five minutes after the second dose, the patient becomes arousable, responds to name, and is able to answer questions. Repeat vitals are BP 121/80, HR 110, RR 15, O2 Sat 98% on room air and ETCO2 at 39 mmHg.
The patient refuses transport to the hospital. He is able to demonstrate decision making capacity and is ambulatory.
This patient has decision making capacity but refuses transport to the hospital. When patients refuse recommended treatment or transport after an overdose, EMS must make Base Contact. The Base should confirm the patient’s decision-making capacity and further discuss the risks of declining transport to the hospital which may convince the patient to agree to further care at the hospital. Many hospitals in Los Angeles County are part of the California Bridge program and offer initiation of Medically Assisted Treatment (MAT) of opioid use disorder with buprenorphine. If the patient ultimately refuses transport, his refusal would be against medical advice given his abnormal vital signs (hypoxia initially and tachycardia post naloxone) and the Base Contact requirement for signing out AMA with a provider impression Overdose/Poisoning/Ingestion (Ref 834, Patient Refusal of Treatment/Transport and Treat and Release at Scene and TP-1200.2, Base Contact Requirements).
This patient qualifies for the Naloxone Distribution Project (NDP) “Leave Behind Naloxone” initiative, as per MCG 1337, Naloxone Distribution by EMS Providers (Leave Behind Naloxone). This MCG was released in the beginning of 2021 and allows EMS providers to distribute naloxone to individuals that are at risk for opioid overdose if a program is established by their provider agency. This is a federally funded program administered by the Department of Health Care Services in California. The program distributes free naloxone to qualifying entities, including EMS provider agencies, for direct distribution to persons at risk for opioid overdose or those in a position to assist persons at risk.
EMS personnel may distribute naloxone, after performing a patient assessment, to individuals who are at risk for opioid overdose or to persons in a position to assist the individual at risk if the at-risk individual meets any ONE of the following criteria:
- The individual was treated by EMS for an opioid overdose with naloxone or supportive care
- The individual’s history or physical exam demonstrates evidence of illicit opioid use (history of intravenous drug use, track marks, needles present, etc.)
- The individual’s history or physical exam demonstrates prescription opioid use (prescribed or recreational)
- The physical environment has opioids or drug paraphernalia present
The naloxone distributed through this program should be separate from the responding unit’s inventory supply. EMS providers who distribute naloxone should perform training for the individual receiving it including:
- How to recognize signs and symptoms of overdose
- Calling 911
- Naloxone administration
- Rescue breathing
- Post-overdose care
Participating provider agencies must track and submit naloxone distribution logs in accordance with NDP requirements. Any agency can apply to obtain naloxone kits free of charge via the NDP through this application: https://www.dhcs.ca.gov/individuals/Documents/NDP-Application.pdf
This patient required transport to the emergency room for ongoing care, however, he opted to refuse transport AMA. In the emergency department, this patient would have been observed for 2 to 6 hours and may have been discharged home after that time if he remained symptom free. Naloxone has a duration of action of 30 to 120 minutes depending on the route of administration and in some cases, the naloxone may wear off before the opioids have cleared the patient’s system, prompting additional doses of naloxone or a naloxone drip. In these cases, patients are often admitted to the hospital. The patient in this case signed out AMA. His friend agreed to monitor him. Paramedics provided training to his friend on naloxone administration and provided the friend with naloxone to use should he observe signs of overdose in accordance with MCG 1337, Naloxone Distribution by EMS Providers (Leave Behind Naloxone).
For those looking for additional education resources highlighting current trends in the opioid crisis, harm reduction strategies, provider self-care, and EMS-driven injury and illness prevention programming, please review the California Opioid Prevention by EMS (COPE) Course. This is a free, online continuing education that offers 2.0 hours CE from an approved California EMS CE provider and can be found at this link: https://caparamedic.org/COPE/.
- Respiratory arrest is the leading cause of death in opioid overdose.
- Naloxone should be administered without delay IN, IM, or IV, and titrated to a respiratory rate ≥ 12 with adequate tidal volume. Contact base for additional doses of naloxone when required.
- For patients whose medical condition improves and who demonstrate decision making capacity and refuse transport, they should be signed out AMA.
- Consider “Leave Behind Naloxone” for any individual at risk for opioid overdose or any person in a position to assist a person at risk if the at-risk individual meets criteria.
- Preventing Emergency Responders’ Exposures to Illicit Drugs https://www.cdc.gov/niosh/topics/fentanyl/risk.html (accessed April 14, 2021)
- Moss MJ, Warrick BJ, Nelson LS, et al. ACMT and AACT Position Statement: Preventing Occupational Fentanyl and Fentanyl Analog Exposure to Emergency Responders. J Med Toxicol. 2017;13:347-351.
Author: Jake Toy, DO